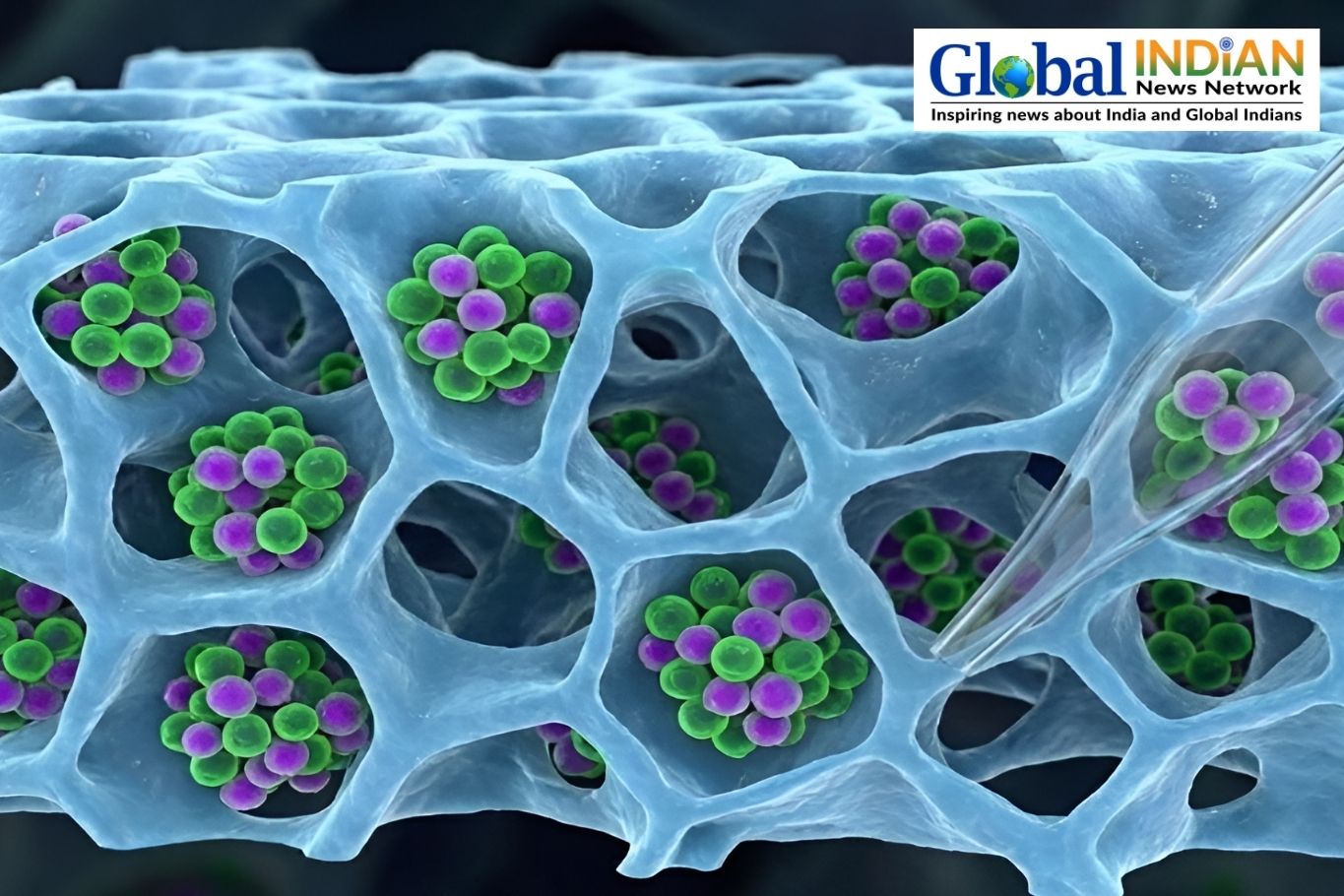
Machine learning algorithms have been harnessed to forecast how gut-produced metabolites bind with receptors in both the gut and the brain. A recent compilation of metabolite-receptor pairs offers researchers insights into the microbiome’s potential role in Alzheimer’s disease.
Researchers at the Cleveland Clinic, Ohio, conducted an extensive evaluation of over 1 million metabolite-receptor shapes to identify potential binding pairs. This method shed light on the biological pathways influenced by these metabolites and revealed the functions of certain receptors.
Lead author Feixiong Cheng, PhD, highlighted the significance of gut metabolites in physiological processes and the challenges in manually deciphering their interactions. Utilizing artificial intelligence (AI), researchers sought to unravel the intricate connections between metabolites and receptors.
The gut’s influence on brain health is underscored by the presence of specific metabolites, indicative of bacterial activity in the gut. Changes in the gut microbiome have been associated with Alzheimer’s disease, potentially impacting brain health through immune mechanisms.
Immunology expert Steve Gendron, PhD, illustrated the communication between the gut and the brain, likening it to a market exchange. Dysfunctional signaling in this communication line may contribute to Alzheimer’s disease progression, akin to using flawed ingredients in baking.
While the immune system’s role in Alzheimer’s disease remains unclear, inflammation has been linked to increased disease risk. Cheng emphasized the challenging nature of Alzheimer’s disease treatment but suggested the potential of the “brain-gut axis” in developing therapeutic interventions.
The identification of metabolite-receptor binding pairs presents an opportunity to explore novel treatment targets for Alzheimer’s disease. By analyzing genetic data and predicting receptor protein shapes, researchers pinpointed lipid-like metabolites with potential therapeutic benefits.
Agmatine and phenethylamine, derived from specific gut bacteria, showed promising effects on reducing tau protein levels associated with Alzheimer’s disease. Cheng emphasized the need for further preclinical studies to validate these findings and explore their efficacy and safety in future trials.
Given the high failure rate of clinical trials for Alzheimer’s disease treatments, Cheng believes their research could pave the way for novel therapeutic avenues. The study’s open-access approach aims to facilitate collaboration and accelerate progress in Alzheimer’s disease research.